Healthcare Leaders: Leveraging Data, Emerging MedTech & Collaboration to Meet the Needs of Underserved Communities
Arthi Chandran
Divisional Vice President of Health Economics and ReimbursementReviews
Understanding and Addressing Healthcare Inequities
When we attempt to address the needs of the underserved within the healthcare system, it's crucial to drive change by understanding the root causes of inequalities. This involves focusing on questions like what makes us different? What drives health care inequities? How does data play a role in addressing these disparities? And how can we make a difference?
With this mindset, we can start to develop strategies that transform patient experiences and curtail healthcare disparities.
Exploring the Causes of Healthcare Disparities
Despite being more similar than different, humans experience healthcare disparities differently. Amongst various ethnicities, racial disparities in healthcare are alarmingly prevalent. For example, people of color such as African Americans or Hispanic Americans often have the highest disease prevalence, with African Americans having a lower life expectancy compared to white Americans.
The question arises - if our genes do not differentiate us, what drives healthcare outcome inequity? The answer lies in the social determinants of health. These determinants include where we work, live, our education, access to healthy food, social support systems, and community culture. Although these factors are influenced by policy and society, they create systemic inequality – disproportionally affecting communities of color.
Empowering Diverse Patient Engagement in Clinical Programs
Understanding the root causes of health inequality is just the starting point. To bridge this divide, the healthcare community needs to go beyond enlisting diverse participants in clinical studies. It involves breaking down barriers via auxiliary services like transportation, education, and health literacy programs within community institutions. Moreover, real-world evidence should form part of our broader learning to ensure technologies contribute as intended.
Patient advocacy is another potent tool for uncovering unmet needs. By amplifying patient voices and forging diverse partnerships, the healthcare community can collectively answer the pressing questions about health disparity.
What Does Good Look Like?
- Understanding the Diversity: A deep understanding of the diverse patient population and the social determinants affecting them can lead to targeted patient support and systemic solutions.
- Collecting and Using Representative Evidence: Rigorous data collection from diverse populations will enable us to validate our solutions, backing them up with robust and representative evidence.
- Influencing Next-Gen Health Care: With these practices in place, we'll improve the solutions we provide while creating a network of learning that continuously mitigates healthcare disparities.
Key Takeaways
1. Understand Your Customer: Recognize the demographic your solution is intended for and ensure that feedback comes from a representative sample.
1. Recognize and Address Bias: Awareness of biases in our methods will enable us to make necessary adjustments.
1. Create Solutions Beyond Product Design: Addressing inequalities sometimes requires strategies beyond the product's design.
1. Plan for Continuous Improvement: Regular reviews can open up avenues for further enhancements in patient engagement.
In conclusion, acknowledging healthcare disparities and implementing ongoing innovative solutions will equip us to serve a diverse patient population better. The continuous dialogue around health equity is vital for ensuring that more and more individuals benefit from medical advances. Though the road is long, the healthcare community's collective effort will ensure progressive change for the underserved.
Video Transcription
So good afternoon and thank you for joining the session. Um Let's just jump right in. I wanted to start today with um with a guidance and that guidance is that to address the needs of underserved.We need to start with understanding, we need to start with the end in mind and kind of work our way backwards. And that starts with questions. So I offer that we need to ask ourselves as well as each other. What makes us different? What drives health care inequities? What role does a fact base and data play in starting to solve for those inequities? And what can we do small things, big things, but what can we do to start driving a difference? And today in in our session, we won't uh talk about a checklist of answers and exactly the formula to fix the problem. But rather I want to um leave everyone listening today with an idea um with a number of ideas, spark thinking um that hopefully you can carry beyond this session. So my name is Aarti Chandran. I'm a chronic disease epidemiologist and a public health professional. I am also the head of health economics and reimbursement for Abbott medical devices and Abbott. Um Abbott's Medical device business. It focuses on addressing some of the world's most complex, most prevalent and costly chronic conditions.
And those include heart disease, cardiac arrhythmias, uh diabetes, um peripheral arterial disease, uh pain, as well as movement disorders. And in my role um at Abbot, I'm responsible for designing pathways to patient access for our pipeline of innovations. Um And to do this, I take into consideration a variety of different things and I look at the world through multiple lenses, I look at um clinical unmet needs. I look at health care utility of our innovations. I also look at the environment and I look at health care policies that can um accelerate access to care, but they can also limit broad access to care. So why, why am I thinking about things from these different angles? Well, it's because we need to design technologies that are resilient to the diverse pathways of health care delivery that we have not only in the United States but around the world, we need to do that so that we truly ensure and all of the patients that we look to serve with our technologies actually have an opportunity from benefiting from the innovations that we're creating for them.
And so asking questions is a really important part of product development, but it's also a really critical part of making sure that the right patient gets the right product or solution at the right time. And so in preparation for today's discussion, I started talking to my colleagues, I started engaging um individuals, leaders in this industry um that touch different phases of product development. Um and really come together to make sure that our ideas turn into products and actually get to our patients.
And I wanted to know what their perspectives on health care in inequity and um managing uh care delivery to the underserved looks like. And in doing so, I um it was most impacted by uh a leader in the clinical development organization who pointed out that humans are more similar than we are different, more similar than we are different. And so we really need to take a step back and question what the root cause of inequity actually is why are certain populations disadvantaged or disproportionately underserved? So I, I'd like to start today by honoring the fact that we are more similar than we are different. So, if race is not um biological, right? If there's no gene that says, um you, you're African American or you're Indian. Um then how do we explain the health care disparities that we see? Why is it that people of color experience illness and experience engagement with health care so differently. And so as we look across chronic disease, you can see here that people of color such as African Americans or Hispanic Americans have some of the highest prevalence of disease.
And what's not shown here is life expectancy. And for African Americans, uh the life expectancy is four years lower than for white Americans and working in the cardiovascular disease space. Um we know that cardiovascular related mortality is decreasing in the United States, but African Americans still have the highest rate of death. So again, if our genes don't differentiate us, then what is driving that inequity in outcomes? So going back to my public health roots, I really appreciated where my research started to take me here, which is social determinants of health. So for those of you who um might not be familiar with this theory, research shows us that um economic and social factors influence um patients health care status. Um they influence our care seeking behaviors and um ultimately, they um can influence the the risk of negative health outcomes.
And so what are these determinants of health? There are many um they could include where we work on a daily basis. They could include where we live, education, access to education, access to healthy food, um the social support systems, our communities, our culture, um and even how we engage with the health care system. And unlike our genetics, um social determinants of health are often driven by policy, they're driven by culture and society. But what's most important is that these factors can create systemic inequality and that systemic inequality disproportionately affects communities of color. So why does this matter?
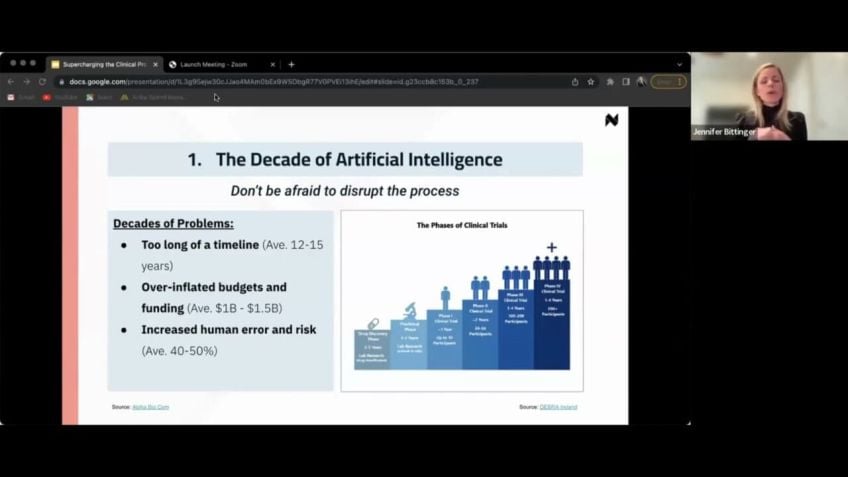
Um how does it relate to data as as well as you know, you know, medical technologies and their role in addressing the underserved. Well, we have to again start at the end and understand the root cause. What is the root cause of inequity and what are the right questions? Are we designing medical technologies or solutions in general that serve the most pressing clinical issues? Probably I can say that, you know, working in this industry for almost 20 years. It's one of the first questions we ask, where are the biggest unmet needs and how do we go after them? So if that's the case, then are we asking ourselves? Well, all the patients that need this particular intervention have an equitable pathway to access. It's an important question because not all of our patients environments are created equally. It's an important consideration, what barriers need to be overcome, to be able to serve the underserved. Also an important question. So in health care, clinical trials are pivotal. They are central to determining whether a product is safe um or whether a product is efficacious. And so we send these off to the, the FDA, we do the work, we send them to the FDA, they look at it and they say yes, this is a safe product to use in humans.
However, uh we know that women and populations of color are systematically underrepresented um in these studies. And so that means that although the studies are Generali zable on a human level, we don't actually look at the utility of these technologies with the same rigor um that we study safety and efficacy and how, so how does this happen? There's a, there's a variety of reasons for why this happens. Um In medical device studies, the cost of that study is often shared by Medicare or uh by commercial insurance. So that in in itself implies that the patient participating in the study most likely gonna have insurance.
So you automatically start to um reduce the proportion of Medicare patients. You're essentially um eliminating the uh you know, individuals who are financially disadvantaged. But if you start to put together, for example, a hardship program, there's still other factors that can lead to that disproportion of patients in your trials. So for example, a clinical trial is gonna follow a very strict protocol uh and that patients must comply to that protocol.
So that means is that you essentially start to eliminate patients that have inflexible work schedules, patients that might not have caregiver support who might not have access to transportation. And the list goes on. So, without designing uh studies that are representative, um it's hard for us to say that we are truly addressing the needs of a heterogeneous population. And we're also again missing that critical piece of evidence that says the way we study um impact in this controlled setting is actually what happens in the real world. So there's multiple factors here that um we can do better at. And that latter piece is really what payers are looking for, right? Uh Health care systems are investing in technologies that we believe will make a difference in the real world. So why aren't we spending an equal amount of dollars to understand whether we're actually hitting that outcome?
It's an opportunity. And so here I just wanna illustrate that um you know, although this, this data is older, I feel like it, it really tells a good story. You can see that clinical trials have historically not represented the diversity of the US population. And in 2011, um we see that African Americans and Hispanic um Americans made up 16 and 12% of the total population respectively. But you can see that they only make up one in 5% of the patients in U SS clinical trials. So think about that since 2011, how many therapies and technologies are not being evaluated on all populations? So here more recently, you see work done by the FDA and they looked at the 53 new drugs that were approved in 2020 that represented 32,000 patients, but 75% of them were white. So this reinforces that disparity in clinical trial participation. And um you know, we saw this recently in our COVID studies. Um but understanding the population that you serve um their unmet needs and the way they seek care is really fundamental to ensuring that we're able to get our product to them and that they are actually um getting the the positive health outcomes that we intend to achieve.
So we've laid out the challenge now. So let's get into opportunities and we can start with clinical trials there. Um You know, there's a, there's a ton that we can do to improve upon um diverse patient engagement with clinical programs. And it again, it starts with those social determinants of health. Let's start removing those barriers um to access to these studies. Um It can be as simple as providing transportation to your site. Um bringing care to a patient's home education. I think health literacy and breaking down cultural barriers that have, you know, put, been put up for a variety of reasons. Not everybody's experience with the health care system is the same and there are communities who um may not want to participate in research for a variety of different reasons. Um Websites might be helpful but they are not the only way to engage with communities working with institutions within communities like churches. Um and you know, trusted, trusted partners within the community, whether it's a nail salon or a barbershop, those are all options and they require work, they require uh creative thinking, but they are all ways in which we can start to bridge the divide.
But moving beyond the clinical programs, we have to keep learning, we should be using real world evidence to really see how patients are engaging with new technologies so that we can really identify uh and eliminate barriers to access and start to ensure that people are benefiting.
And again, in the ways that we intend, we need to give patients a voice. Patient advocacy is an incredibly powerful tool, helping patients articulate what their needs are very specifically and helping us understand where there are populations that are um underserved by our technologies.
We also need to partner. Um It can't just be one individual, one group that's asking these questions, but we need to make it a norm. Um Making sure that all of us are asking these questions, answering these questions and then subsequently investing in addressing these questions.
Um so that we can start to make incremental movement forward. And so what is good look like? What happens when we start to do these things, right? And we start to do them more often. Well, you know, I think um just by understanding the people that we are trying to serve better and the the diversity of the people that we are trying to serve better, the way they engage with their health care systems, the social determinants that govern the way you and I engage with the health care system.
It allows us to um be more targeted in how we support our patients. But that volume of information we collect by collectively thinking differently, will allow us to systematically identify things that we should constantly be solving for that. We're not solving for today. So we will learn together by asking these questions and we'll start to see that our evidence, whether it's clinical evidence or whether it's real world data that we're collecting, it's gonna be more representative and we're gonna have information that validates each other and creating really a network of learning um that allows us to solution for the individuals who today are underserved and hopefully tomorrow are not.
And that's where our next gen health care um is going to be impacted, right? So if we start doing these things, right, we're going to start to improve the solutions that we bring to the table, but also how we bring them to the table. And those are the types of things that are gonna start to be more measurable. And so, you know, I think in, in terms of takeaways here, um I believe that these takeaways are true regardless of the type of product or solution that we're actually bringing to the marketplace. Um One just understanding your customer understanding who we are trying to serve and making sure that um it's a representative sample of who we're trying to serve. I think biases are always going to exist. Um They're always gonna exist in our methods. And so it's just, it's the nature of the research we do. It's the nature of our systems today. So we shouldn't be afraid to talk about it. Um We should be open we should have an open dialogue around bias and identify ways to compensate for that bias. And by doing that, we will make incremental improvements towards a better outcome. I think we have to know that we can't always solve for inequity using a design of a technology. So we have to think about design plus, um we have to plan to do more beyond the product to make sure that our product is actually serving the population, the communities that we wanna serve.
And I think one thing that we can all rely on or count on is continuous improvement. We should plan on it. We should plan on continuous improvement and always asking these questions and always um improving the way we engage. So I offer you these things. Um I hope that um you do walk away from this session with new ideas, something to chew on. Um but feel free to reach out to me with any questions um or comments if you want to continue this discussion. Thank you.



No comments so far – be the first to share your thoughts!